Medicare Advantage, Medicaid Managed Care, Health Insurance Marketplace® and commercial insurance plans now cover covering nearly 80% of Americans. These payers require Prior Authorization (PA) for most procedures and many medications, a process which has negatively impacted both practitioners and patients, including (and maybe in particular) patients with chronic wounds…
- The Kafkaesque Challenge of Medicare Advantage Prior Authorization – Caroline Fife M.D.
- Late Night Thoughts on HBOT Prior Authorization – About the Centers for Medicare & Medicaid Services (CMS) Daily Digest Bulletin – Caroline Fife M.D.
…and has been described by practitioners as an “overwhelming burden.” Maybe now there is reason to hope.
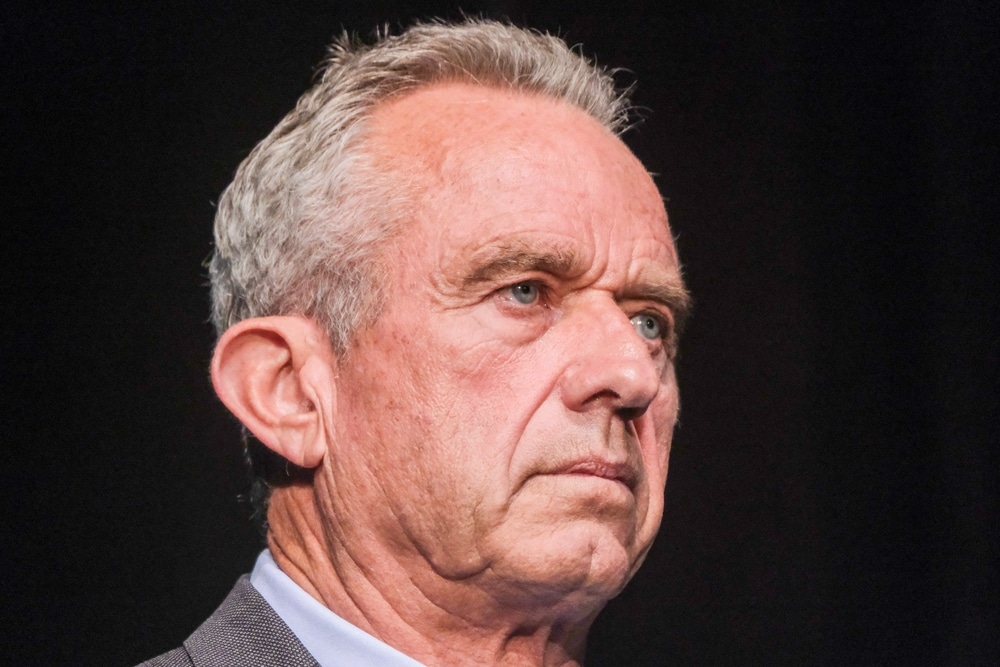
On June 23, 2025, Health and Human Services (HHS) Secretary Robert F. Kennedy, Jr. and Centers for Medicare & Medicaid Services (CMS) Administrator Dr. Mehmet Oz met with industry leaders to discuss their pledge to streamline and improve the prior authorization processes for these payers. Six Key reforms to the PA process have been promised:
- Standardize electronic prior authorization submissions using Fast Healthcare Interoperability Resources (FHIR®)-based application programming interfaces.
- Reduce the volume of medical services subject to prior authorization by January 1, 2026.
- Honor existing authorizations during insurance transitions to ensure continuity of care.
- Enhance transparency and communication around authorization decisions and appeals.
- Expand real-time responses to minimize delays in care with real-time approvals for most requests by 2027.
- Ensure medical professionals review all clinical denials.
Their commitments reinforce the role of CMS in monitoring outcomes and promoting accountability. Companies represented at the roundtable included Aetna, Inc., AHIP, Blue Cross Blue Shield Association, CareFirst BlueCross BlueShield, Centene Corporation, The Cigna Group, Elevance Health, GuideWell, Highmark Health, Humana, Inc., Kaiser Permanente, and UnitedHealthcare.
Additional Resources:
- Artificial Intelligence vs Augmented Intelligence in Prior Authorization Denials – Caroline Fife M.D.
- How to Prevent Improper Use Without Costly, Time Sucking Prior Authorization – Caroline Fife M.D.
- Newsflash: Bi-Partisan Agreement on Something! Prior Authorization is Not a “Benefit” – Caroline Fife M.D.
- Physicians: Prior Authorizations are an Overwhelming Burden – Caroline Fife M.D.
- Insurers Continue AI Claims Automation Despite Legal Challenges – Caroline Fife M.D.
- Will “Just Say No” Be the Future of Cellular Product Coverage? – Caroline Fife M.D.