Wound Care Quality Benchmarking
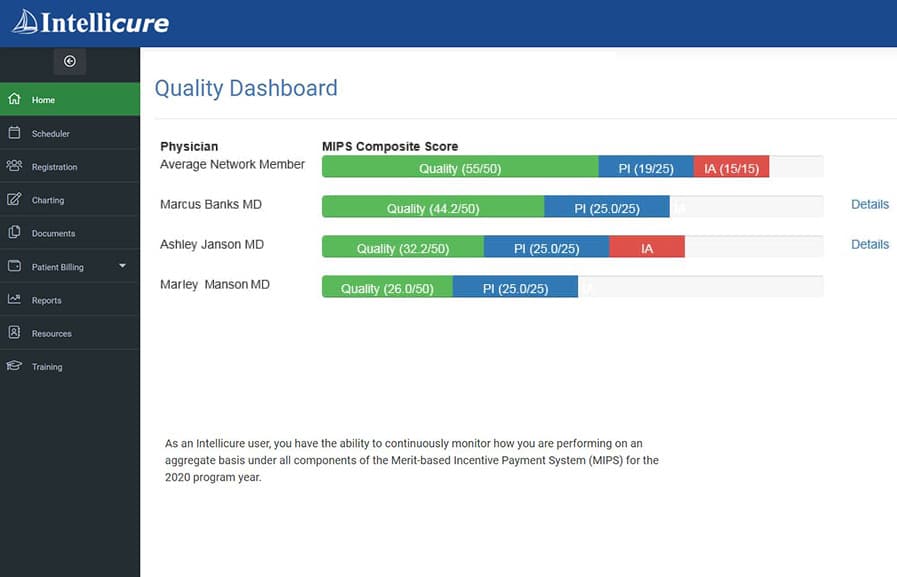
Intellicure’s Quality Dashboard shows clinicians’ wound care quality scores benchmarked against national averages.
Better Quality Scores Lead to Better Reimbursements. It’s no secret that CMS and private payors adjust their reimbursements based on Quality Payment Programs such as MIPS. Better wound care quality scores result in better outcomes, robust documentation, and more complete, accurate payments.
Intellicure’s Quality Dashboard is the wound center’s ace in the hole. The Quality Dashboard benchmarks the wound center’s physicians’ quality measure performances against national averages, enabling the wound center to achieve the highest possible MIPS scores and optimal wound care reimbursements.
Physicians using Intellicure always outperform their peers because they’re utilizing wound care specific quality measures recognized by CMS and authored by the US Wound Registry, which are built into Intellicure’s wound care software.
To further the ascent to quality care, the wound center manager can select the quality measures they want to be benchmarked against.
See Intellicure's Quality Dashboard in Action!
Schedule a live demonstration of Intellicure's award-winning wound care software by submitting the form below. Your information will never be sold or shared.
Intellicure's leading wound care software
delivered how you need it.
Use Intellicure as a Complete
Wound Care EHR
Intellicure's wound care software includes full-service EHR components, like scheduling, registration, charting, and billing and reporting tools. IntellicureEHR interfaces with any hospital EHR. It's an optimal solution for any wound care center or private practice looking for a fast, compliance-focused wound care EHR. IntellicureEHR it's usable on any device and can be logged in from anywhere.
Use Intellicure as a SMART App
inside the Hospital's EHR
Intellicure's wound care charting module is now available as an interoperable SMART app inside your hospital's EHR, like Cerner, Epic, Meditech, or any EHR provided it uses FHIR, the latest HL7 standard. This option delivers Intellicure's industry-leading charting software as part of your EHR's workflow, which is ideal for wound centers using the hospital's EHR.
Have questions? Call (800) 603-7896 to speak with a wound care expert at Intellicure, or click here to schedule a live demonstration of Intellicure.
“I love seeing the Quality Dashboard every time I log into Intellicure.”
— Pam McSweeney, Program Director
Wound and Hyperbaric Medicine Center at Sweeny Community Hospital