These proposals are in a comment period until June 8, 2024. Any interested stakeholder may submit comments to share their feedback on these proposals.
Blog Posts by Jeffrey D. Lehrman, DPM, FASPS, MAPWCA, CPC, CPMA
MIPS Quality Measure #130 Documentation
Too many providers are under the impression that merely documenting the patient’s medication list satisfies the performance of this measure, and it does not.
G2211 Documentation
Last month’s blog explained HCPCS G2211, its appropriate use, and inappropriate use. HCPCS G2211 -...
New Coding When Caring For a Complex Condition
G2211 should be added to an office or other outpatient evaluation and management CPT® code. It should never be submitted alone.
MIPS Revenge!
The MIPS program has continued to evolve with penalties increasing and the participation threshold needed to avoid a penalty also increasing.
CPT® Change for 2024
There are major changes to CPT coding associated with noncontact near-infrared spectroscopy.
ICD-10 Changes
A new ICD-10 Clinical Modification (ICD-10-CM) code set took effect October 1, 2023. In this new code set, there are many code additions, deletions, and modifications.
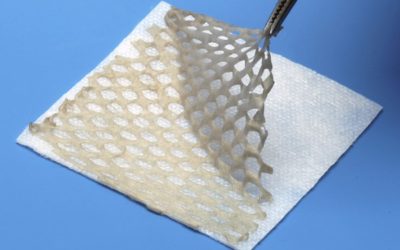
JZ Modifier Use With Skin Substitutes
CMS has issued guidance requiring the use of Modifier JW on all claims for biologicals from single-dose containers that are separately payable under Medicare Part B when there are unused / discarded amounts.
Ulcer Debridement & Total Contact Cast Application
We cannot submit CPT®[1] coding for both ulcer debridement and total contact cast application when both are performed for the same ulcer at the same encounter.
New Surgical Treatment of Nails Policy
This policy is being contested by multiple stakeholders, including the American Podiatric Medical Association.
New CTP Coding Requirement
Effective July 1, 2023, providers must report the JZ modifier when an entire skin substitute product is applied to a Medicare Part B beneficiary and there is no waste.
New Suture / Staple Removal CPT® Codes
These CPT codes can be used if the patient is not in a global period for the provider who removes the sutures / staples.
Expansion of Lymphedema Treatment
The CY 2024 Final Home Health Prospective Payment System Final Rule contains significant changes that expand coverage for lymphedema treatment.
More Exciting E&M Changes!
The process by which office and other outpatient evaluation and management (E&M) levels (CPT® 99202 – 99215) are selected was changed by the AMA CPT® Editorial Panel effective January 1, 2021.
Consolidation of E&M Services in 2023
Effective January 1, 2023[1], under the guidance of the AMA CPT Editorial Panel, many evaluation...
Place of Service for “Observation” Status Patients
It is important to know if the patient is in the hospital under “observation” status or “inpatient” status because this affects CPT® code selection.
The Importance of CPT® 99024
Yes, specialists who are not the admitting / primary physician may submit CPT 99304 in certain situations.
Zero Day Postoperative Global Periods
If you perform either or both of the procedures represented by CPT 28820 and 28825, be sure to code appropriately for the services performed during the postoperative global period.
Wound Repair CPT® Codes
When it comes to CPT® coding, wound repair is typically classified as simple, intermediate, or complex.
Pressure Ulcer Versus Pressure Injury ICD-10-CM Coding
When documenting and coding skin changes that result from prolonged pressure, it is important to differentiate between a pressure “ulcer” and a pressure “injury.”
Is Collagen Billable Following Elective Procedures?
Some providers dispense surgical dressings to patients and submit coding for the dressings to third party payers in exchange for payment.
Can Specialists Submit CPT® 99304?
Yes, specialists who are not the admitting / primary physician may submit CPT 99304 in certain situations.
Appropriate Use of CPT® 11755
This CPT is often used incorrectly. Fortunately, clarity is provided in the form of a CPT Assistant article published in December, 2002.
Coding During the Postoperative Global Period
Many wound care – related procedures, including some amputations and certain incision and drainage services, carry with them a 10 or 90-day postoperative global period.
Assessing Malnutrition During the Wound Healing Process
Assessing a patient’s nutritional status during the wound healing process is of tremendous importance. Here are some lists for patients.
Diabetic Foot Ulcer Coding – Diabetes Awareness Month
November is Diabetes Awareness Month. For those that treat diabetic foot ulcers, this is a good opportunity to ensure your diabetic foot ulcer coding is accurate.
What Exactly is a Separately Identifiable Evaluation & Management?
When a significant and separately identifiable E&M and a procedure are both performed, the documentation of the encounter must clearly reflect two separate services with no overlap in work between the E&M and the procedure.